Education
CVP Physiology
Central Venous Pressure (CVP) is the clinical measurement of right atrial pressure. It is used to evaluate the adequacy of circulating blood volume and cardiac preload. Central venous pressure is comprised of the pressure generated by the volume of blood returning to the right atrium and the pressure adjacent to the heart, called juxta-cardiac pressure. The gradient between mean systemic filling pressure and CVP creates venous return and cardiac output 1.
Venous return is the rate that blood returns to the heart. Mean systemic filling pressure, right atrial pressure, and vascular resistance all play a key role in venous return. Cardiac output correlates with the function and performance of the heart. Ventricular afterload, autonomic tone, and many intrinsic factors affect cardiac output.
Any factor that causes a change in venous return and/or cardiac output can greatly influence CVP. An elevated CVP may be due to an impediment to venous return, hyperinflation, venous return has exceeded the limit of cardiac accommodation, dysfunction in the right heart or obstruction to right ventricular outflow - causing retention of blood, renal failure, or hepatic dysfunction. A lower CVP could be a response to venodilation - causing low venous return, volume loss, sympatholysis, or from any cardiac function that encourages the ejection of blood 1-4.
Due to the fact that CVP is very responsive to any change in venous return or cardiac output, it has shown to be an important measurement to integrate with other monitoring techniques, to better evaluate the patient's hemodynamic instability and to confirm a preliminary diagnosis. It has been used in the ICU for hemodynamic intervention, and bedside for interpretation of a bedside echocardiogram 4.
Current Method
Currently the common practiced method for attaining CVP is by invasive central venous catheter. Many risks and complications are associated with central venous catheters therefore it would be an attractive option to have a non-invasive technique. Mespere LifeSciences has developed a novel device to continuously monitor CVP non-invasively.
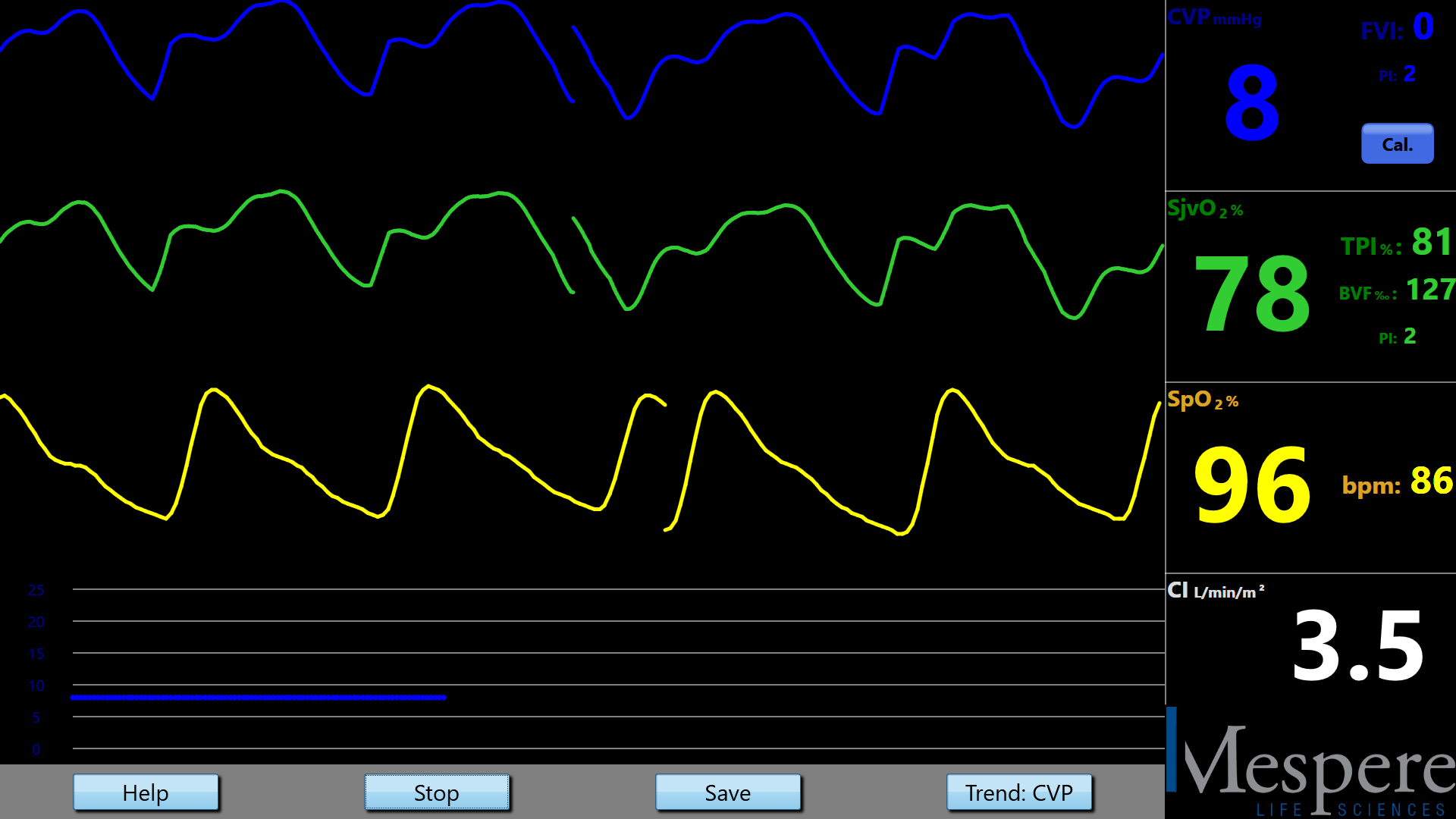
The Mespere VENUS 2000 CVP system will help make the physical examination of CVP an easier and reliable process for the physician. In addition, the Mespere VENUS 2000 CVP system will have the additional benefits of allowing physicians to continuously asses CVP over a period of time and to observe the plethysmographic waveform, a feature not available with physical examination.
Interpreting a Change in CVP Measurement
Normal range for CVP is between 4-12 cmH 2O or 3-8 mmHg. A CVP reading outside of this range should be monitored, and appropriate measures should be taken to get the CVP back into the normal range.
Accuracy of the Mespere VENUS 2000 CVP System Compared to Catheters
Current risks involved with taking continuous CVP measurements, are catheter placement and maintenance. Catheters are susceptible to conflicting results due to, the rate that fluids are introduced, head positioning, and correct tip placement 5. The current precision for commonly used catheters is -0.1±3.5 cmH 2O 6. Contrary to catheters, the Mespere VENUS 2000 CVP is not susceptible to these risks since it is non-invasive, and there is no placement or insertion of a catheter. The accuracy and precision of the Mespere VENUS 2000 CVP is ± 1.35 cmH 2O or ±1 mmHg, therefore it is more precise than the current traditionally practiced method for attaining CVP.
Clinical Applications of Non-Invasive CVP
The Mespere VENUS 2000 CVP system is indicated for individuals to measure hemodynamic cardiac pressures in the human body to allow physicians to better understand cardiovascular health. The Mespere VENUS 2000 CVP system should be used by health care professionals as a non-invasive, spot-checking and/or continuous monitoring tool for physical assessment of central venous pressure (CVP) of an individual. This is done via an adhesive neck sensor placed over the external jugular vein. The device is intended for use in hospital and clinical environments.
The Mespere VENUS 2000 CVP System is ideal for preload and volume status assessment and monitoring for patients with congestive heart failure, sepsis, renal failure, congenital heart disease etc. It can be used in a variety of settings including Emergency Departments, Intensive Care Units, Heart Failure Clinics, and Long Term Care Facilities.
References
- Berlin, D.A., Bakker, J. (2015) Starling curves and central venous pressure. Critical Care, 19:55. DOI 10.1186/s13054-015-0776-1
- Jacobsohn, E., R. Chorn, and M. OConnor, The role of the vasculature in regulating venous return and cardiac output: historical and graphical approach. Canadian Journal of Anaesthesia-Journal Canadien D Anesthesie, 1997. 44(8): p. 849-867.
- Funk, D.J., E. Jacobsohn, and A. Kumar, The role of venous return in critical illness and shock-part I: physiology. Crit Care Med, 2013. 41(1): p. 255-62.
- Kenny, J-E.S., ICU Physiology in 1000 Words: In Defense of the Central Venous Pressure. Crit Care Med, 2014.
- Chatterjee, K. (2007) Physical Examination. In E.J. Topol (Ed.), Textbook of Cardiovascular Medicine (3rd Edition ed., pp. 1993-224). Philadelphia: Lippincott Williams & Wilkins
- Thalhammer, C., Ashwanden, M., Odermatt, A., Baumann, U., Imfeld, S., Bilecen, D., Marsch, S., Jaeger, K., Noninvasive Central Venous Pressure Measurement by Controlled Compression Sonography at the Forearm. Journal of the American College of Cardiology, 2007. 0735-1097
For a PDF version, please download this document.
Physiology and Venous Oxygen Saturation
Venous oxygen saturation (SvO 2) is a measurement used to describe the balance between oxygen delivery and consumption in the brain. SvO 2 has been studied comprehensively, since it has shown to be an improved measurement over the traditional methods (heart rate, blood pressure and central venous pressure). Monitoring jugular venous oxygen saturation (SjvO 2) has been occurring for many decades and has shown to have useful clinical applications for neurosurgical procedures, cardiovascular procedures, head injuries, and sepsis patients.
Monitoring jugular venous oximetry allows clinicians to make more accurate adjustments, in order to improve the patient's wellbeing and will result in better long term outcomes.
Current Method
In the past monitoring involved the use of co-oximetry laboratory analysis and fiber optic technology. Currently the most common device used are fiber optic catheters. Fiber optic catheters are an invasive method. The Mespere VO 100 Jugular Venous Oximetry is a noninvasive continuous jugular venous oxygenation monitoring system, which uses near infrared spectroscopy to measure venous hemodynamics without the need for invasive catheterization.
Interpreting a Change in Venous Oxygen Saturation
The normal range for SjvO 2 is 60-80%, below 60% usually indicates that there is a low oxygen delivery, and above 80% indicates that there is low consumption. When monitoring a patient, clinicians should look for changes of ±5-10% for a period of 5 minutes of longer. If this occurs, that it is an indication of a change in oxygen consumption or demand 3. Jugular desaturation commonly occurs in patients with traumatic brain injury 4, cardiac surgery patients 4, and patients that are comatose.
Accuracy of the Mespere VO 100 Jugular Venous Oximetry Compared to Catheters
Current risks involved with taking a SjvO 2 reading, are catheter placement and maintenance. Catheters are susceptible to conflicting results due to, the rate that the blood is withdrawn, head positioning, and correct tip placement 1. The current precision for commonly used fiber optic catheters, is ±4.41% 2. Contrary to fiber optic catheters, the Mespere VO 100 Jugular Venous Oximetry system is not susceptible to these risks since it is non-invasive, blood is not withdrawn and there is no placement or insertion of a catheter. The accuracy and precision of the Mespere VO 100 Jugular Venous Oximetry is ±2.00%, therefore it is more precise than the current SjvO 2 continuous monitoring methods.
Clinical Applications of Venous Oxygen Saturation
Monitoring jugular venous oxygen saturation (SjvO 2) has been occurring for many decades and has useful clinical application for neurosurgical procedures, cardiovascular procedures, head injuries, and sepsis patients. Continuous monitoring of venous oxygenation, has shown to be a valuable measurement for clinicians. It allows them to monitor the balance between oxygen delivery and consumption. The Mespere VO 100 Jugular Venous Oximetry is a non-invasive continuous jugular venous oxygenation monitoring system that is more accurate, precise, and has far less risks than most commonly used fiber optic catheters.
The Mespere VO 100 Jugular Venous Oximetry is ideal for use in Emergency Departments, Intensive Care Units and in Anesthesia.
References
- Holly C.G., Matta B.F., Lam A.M., Mayberg T.S., Accuracy of Continuous Jugular Bulb Venous Oximetry during Intracranial Surgery. J. Neurosurgical Anesthesiology 1995:7(3):174-7
- Mahajan A, et al. An Experiment and clinical evaluation of a novel central venous catheter with integrated oximetry for pediatric patients undergoing cardiac surgery. International Anesthesia Research Society 2006; 16:1257-63
- Frazier J., Theory and Clinical Application of Continuous Fiberoptic Central Venous Oximetry (ScVO2) Monitoring Edwards Lifesciences
- Roberson CS, Gopinath SP, Goodman JC, et al. SjvO 2 monitoring in head-injured patients. J Neurotrauma 1995;12:891-6
- Croughwell N. Warming during cardiopulmonary bypass. Ann Thorac Surg 1992;53:827-32
For a PDF version, please download this document.
Facts about Sepsis
- Worldwide incidence of sepsis is estimated to be 19 million cases per year 1.
- Between 28-50% of people diagnosed with sepsis die 2.
- Most expensive condition treated in U.S. hospitals, costing $20 billion in 2011 and increase on average annually by 11.9% 3.
- Mortality from sepsis increases 8% for every hour that treatment is delayed. As many as 80% of sepsis deaths could be prevented with rapid diagnosis and treatment 4.
- 80% of patients diagnosed with sepsis developed the condition outside the hospital 5.
What is Sepsis
Sepsis is a life-threatening illness caused by the body's response to an infection. Sepsis can be broken down into three core stages.
- Sepsis: chemicals of the immune system reach the bloodstream and cause inflammation throughout the body.
- Severe Sepsis: infection disrupts blood flow to the brain or kidneys, leading to organ failure.
- Septic Shock: patient's blood pressure drops significantly causing respiratory, heart, or organ failure which could result in mortality 6.
Current Common Practice
Sepsis must be treated as an emergency. Aggressive fluid resuscitation must be performed to restore tissue perfusion in order to prevent organ dysfunction.
- Within 3 Hours: aggressive fluid resuscitation by administering antibiotics and intravenous fluids to the patient, approximately 30mL/kg
- Within 6 Hours: in the case of blood pressure remaining low despite initial fluid resuscitation, central venous pressure and central venous oxygen saturation should be measured
- Within 12 Hours: essential to diagnose or exclude any source of infection
Fluid Overload
If too much fluid is administered, then fluid overload can occur and cause further complications. Clinical studies have shown that fluid overload can lead to hypertension, peripheral edema, pulmonary edema, respiratory failure, and increased cardiac demand 4,7,8 <.
Mespere LifeSciences Solution
Mespere LifeSciences introduces the first-ever monitoring systems that use near infrared spectroscopy to accurately measure venous hemodynamics without the need for invasive catheterization. Our innovative and cost-effective solutions can be used to ensure that patients are receiving the appropriate fluids in a timely manner.
VENUS 2000 CVP - Mespere LifeSciences VENUS 2000 CVP is a non-invasive and continuous central venous pressure (CVP) monitoring system. With the use of our product, healthcare professionals can now easily and efficiently monitor fluid levels during resuscitation to avoid overload.
VO 100 Jugular Venous Oximetry - Mespere LifeSciences VO 100 Jugular Venous Oximetry is a non-invasive and continuous monitoring system for jugular venous oxygen saturation (SjvO 2). Our product allows healthcare workers to monitor the effectiveness of fluid resuscitation for tissue re-perfusion and make sure that the appropriate treatment is being provided to the patient.



Reference
- Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet 2010;376:1339-46.
- Wood KA, Angus DC. Pharmacoeconomic implications of new therapies in sepsis. PharmacoEconomics. 2004;22(14):895-906.
- Torio CM, Andrews RM: National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011: Statistical Brief #160. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet] Rockville (MD): Agency for Health Care Policy and Research (US) 2006-2013
- Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M.: Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006 Jun;346(6):1589-96.
- Making Health Care Safer. CDC Vital Signs. Aug 2016
- Fitch, S. J., & Gossage, J. R. (2002). Optimal Management of Septic Shock. PostGraduate Medicine , 111 (3). Retrieved June 29, 2016, from http://www.healthline.com/health/septic-shock#Overview1
- Alsous F, Khamiees M, DeGirolamo A, Amoateng-Adjepong Y, Manthous C. Chest. (2000) Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study. Jun; 117(6):1749-54.
- Marik, P.E., Linde-Zwirble, W.T., Bittner, E.A. et al. Intensive Care Med (2017). doi:10.1007/s00134-016-4675-
For a PDF version, please download this document.
Telemedicine
Mespere LifeSciences noninvasive and continuous monitoring systems can be used in long term care and heart failure clinics to remotely diagnose and treat patients.
For a PDF version, please download this document.
Congenital Heart Disease
The Fontan procedure has been performed on pediatric patients to treat a number of serious congenital heart defects, many requiring a single-ventricle repair. Many patients who have undergone this procedure begin to experience new problems as they develop into adulthood. They will need to receive care in new areas other than the pediatric cardiology. This group of patients may now receive care at adult cardiology, cardiac surgery, emergency departments, cardiac clinics and other departments as they encounter problems. It is important that the physicians in these settings understand the complications and problems that arise as a Fontan procedure patient reaches adulthood. Central venous pressure is an important measurement that physicians monitor in Fontan procedure patients. Currently there are no accurate ways to get a non-invasive estimation of central venous pressure.
Mespere has developed a novel developed a novel device, VENUS 2000 CVP monitoring system, for non-invasive, easy and quick to use, with much lower cost. This device may potentially bring multiple benefits to the clinics including improving patient outcome, earlier screening for timely intervention, and reducing cost.
Heart Failure
Patients with fluid sensitive conditions such as acute heart failure frequently present to the ED requiring urgent medical care. The frequency and potential lethality of these conditions, it is imperative that physicians develop accurate methods of determining which course of treatment is best for their patients.
Acute HF represents the opposite end of the preload continuum from severe sepsis and septic shock as these patients typically present with fluid overload and require diuresis or other measures to reduce pulmonary congestion that results from increased preload. Traditionally the sickest of these patients were managed by placing a Swan-Ganz catheter in order for clinicians to gain insight into the hemodynamics of these patients. However, because of the adoption of less invasive techniques the Swan-Ganz catheter has fallen out of use 1. Research has demonstrated that when physicians do not use any type of hemodynamic monitoring technology, they often miss the mark completely in assessing individual patients underlying hemodynamic state 2.
The ability to non-invasively, accurately, and continuously measure CVP to assess the preload statues of ED patients could lead to its inclusion into existing protocols (similar to EGDT), or the development of novel protocols for the treatment of patients with fluid sensitive conditions. The VENUS CVP device has the best of all features given its non-invasive application, and continuous monitoring capabilities. The data provided by the device can be used by physicians.
Reference
- Marik PE. (2013) Obituary: Pulmonary Artery Catheter 1970-2013. Annals of Intensive Care 3:38
- Nowak RM, Sen A, Garcia AJ et al. (2011) The Inability of Emergency Physicians to Clinically Estimate Underlying Hemodynamic Profiles of Acutely Ill Patients. Amer J EM; May 11
For more information, please read this document.
Fluid Challenge
Administering fluids via intravenous is a routine procedure for many patients. Fluid Challenge is an important dynamic test that is completed by administering fluids while simultaneously testing the preload reserve of the patient. It is used as a method to recognize patients who would benefit from an increase in intravenous volume. By conducting a fluid challenge, it reduces the risks associated with fluid overload which would occur when administering excessive fluid during therapy 1.
Current Common Practice
The current common practice to determine a patient's response to fluid is done by monitoring cardiac output 1. A Fluid Challenge is conducted by administering a fluid bolus, and monitoring whether the patient is responsive by looking for a change in cardiac output. The most common method for monitoring cardiac output is with ultrasound. The limitations with the use of ultrasound is that it is based on imaging, therefore cannot be used as a continuous monitor
Mespere Solution
Jugular venous oxygen saturation (SjvO 2) is the amount of oxygenated blood in the jugular vein. It is affected by four factors; cardiac output, hemoglobin, oxygenation, and oxygen consumption 2. Based on Fick's Principle, the trending change of oxygen saturation in the external jugular vein is proportional to the trending change of cardiac output.
Mespere LifeSciences has developed the VO 100 Jugular Venous Oximetry which continuously monitors SjvO 2 non-invasively. The VO 100 Jugular Venous Oximetry can be used to monitor the cardiac output trend based on Fick's Principle. The advantages of the VO 100 Jugular Venous Oximetry is that it is; continuous, cost effective, highly sensitive, easy to use, and non-invasive.
Reference
- Cecconi, M., Parsons, A.K., Rhodes, A. (2011) What is fluid challenge? Curr Opin Crit Care 17:290-205.
- Frazier, J., Theory and Clinical Application of Continuous Fiberoptic Central Venous Oximetry (ScVO 2) Monitoring Edwards LifeScience
Fluid Assessment & Monitoring
Administering fluids via intravenous is routine procedure for many patients. The amount of fluid, composition and the administration rate differs between patients. If one of those factors is incorrect it could have harmful effects on the patient. The assessment and monitoring of fluid status can reduce complications and will improve the patient's wellbeing.
Current Method
Currently guidelines are available to be followed during fluid administration and fluid therapy. Many of these guidelines suggest using central venous pressure (CVP) as a measurement to guide fluid status and management. Surveys have shown that 90% of intensivists use CVP to monitor fluid resuscitation in patients 1.
Central venous pressure (CVP) is the clinical measurement of right atrial pressure. It is used to evaluate the adequacy of circulating blood volume and cardiac preload. Any factor that causes a change in venous return and/or cardiac output can greatly influence CVP. An elevated CVP measurement could be due to fluid overload which would exceed the limit of cardiac accommodation. Low venous return or volume loss of fluids, would result in a decreased CVP measurement 2-5.
The current common practice for attaining CVP is by invasive central venous catheter. There are many risks and complications associated with central venous catheters, therefore it would be an attractive option to have a non-invasive option. Mespere Lifesciences has developed a device to continuously monitor CVP non-invasively.
Mespere Solution
The Mespere VENUS 2000 CVP system is a non-invasive, continuous monitoring tool for the assessment of fluid status. During the administration of fluids the Mespere VENUS 2000 CVP system will provide continuous measurements of CVP. This monitoring could be used to ensure that the patient is being administered fluid at the appropriate rate and quantity. The Mespere VENUS 2000 CVP system is easy to use, and provides continuous, non-invasive monitoring at a low cost.
Reference
- Marik, P.E. (2010) Hemodynamic Parameters to Guide Fluid Therapy. Transfusion Alter Transfusion Med. 11(3):102-112
- Berlin, D.A., Bakker, J. (2015) Starling curves and central venous pressure. Critical Care, 19:55. DOI 10.1186/s13054-015-0776-1
- Jacobsohn, E., R. Chorn, and M. OConnor, The role of the vasculature in regulating venous return and cardiac output: historical and graphical approach. Canadian Journal of Anaesthesia-Journal Canadien D Anesthesie, 1997. 44(8): p. 849-867.
- Funk, D.J., E. Jacobsohn, and A. Kumar, The role of venous return in critical illness and shock-part I: physiology. Crit Care Med, 2013. 41(1): p. 255-62.
- Kenny, J-E.S., ICU Physiology in 1000 Words: In Defense of the Central Venous Pressure. Crit Care Med, 2014.
For a PDF version, please download this document.
Cerebral Tissue Perfusion
Continuous monitoring of venous oxygenation, has shown to be a valuable measurement for clinicians. It allows them to monitor the balance between oxygen delivery and consumption. Traditionally, Jugular Venous Oxygen Saturation (SjvO 2) is a measurement of the amount of oxygen in the venous blood taken from a catheter inserted into the jugular venous bulb. The SjvO 2 reflects the amount of oxygen left over after the brain has used what it needs. SjvO 2 is the percentage of oxygen bound to hemoglobin (oxygen saturation). If the SjvO 2 falls below 55%, it suggests that the blood flow to the brain is not enough to meet the brain's oxygen requirements, causing the brain to extract a greater percentage of oxygen from the blood.
A rise in SjvO 2 can also be important. If the brain injury becomes so severe that the brain is unable to extract oxygen, the SjvO 2 will rise. In brain death, when the brain is no longer capable of extracting any oxygen, the SjvO 2 will equal the SaO2.
Monitoring of jugular venous hemoglobin oxygen saturation (SjvO 2) is not a new technique. This monitoring method has been used since the 1940s. What has changed in recent years is the method of monitoring SjvO 2. In early studies, a blood sample was obtained by direct needle puncture of the superior jugular bulb by inserting the needle one centimeter anterior and inferior to the mastoid process. In general the technique was used either to calculate the arteriovenous difference in oxygen tension and hemoglobin saturation in neurosurgical intensive care unit (NICU) or intraoperatively in patients undergoing carotid endarterectomy (CEA). During CEA, a single sample of blood from the jugular bulb was analyzed shortly after occlusion of the ipsilateral internal carotid artery. It was used as a monitor of adequacy of collateral cerebral circulation in order to determine the need for placement of an arterial shunt.
The most common method to monitor SjvO 2 is to insert a double or triple lumen catheter to monitor SjvO 2. Blood draws are taken and analyzed by a Co-Oximeter. Newer technologies use a fiberoptic catheter that allows for continuous measurements of central venous oxygen saturation. The Mespere VO 100 Jugular Venous Oximetry is a non-invasive continuous jugular venous oxygenation monitoring system that is more accurate, precise, and has far less risks than most commonly used fiber optic catheters.
- Non-invasive measurement of right atrial pressure by near-infrared spectroscopy: preliminary experience. A report from the SICA-HF study
- Starling Curves and Central Venous Pressure. Berlin DA, Bakker J. Crit Care. 2015; 19:55
- Cerebral Monitoring: Jugular Venous Oximetry. Schell RM, Cole DJ. Anesth Analg. 2000; 90:559-66
- Comparison between noninvasive measurement ofcentral venous pressure using near infrared spectroscopy with an invasive central venous pressure monitoring in cardiac surgical Intensive Care Unit. Sathish N, et al, Ann Card Anaesth [serial online] 2016 [cited 2016 Jul 12 ];19:405-409
- Non-Invasive Measurement of Right Atrial Pressure by Near-Infrared Spectroscopy: Preliminary Experience. Poster abstract from SICA-HF Study. Pellicori et al
- Validation of VENUS 1000 CVP System against invasive right heart catheter(RHC). Koelling et al. Journal of Cardiac Failure, 2013; 19(8):S51


